Background: With a narrow therapeutic range, warfarin use needs to be closely monitored to minimize the risk of bleeding or thrombosis. Point-of-care (POC) International Normalized Ratio (INR) tests using finger stick blood samples provide instantaneous results and improve testing efficiency; however, the test accuracy of POC-INR may be affected by various factors such as anemia (1, 2). Thrombosis and warfarin use are prevalent in patients with sickle cell disease (SCD) (3), but evidence on the accuracy or correction of POC-INR in this patient population is lacking. This study evaluates correlation of POC-INR to clinical laboratory INR (CL-INR) in patients with SCD.
Methods: POC-INR and CL-INR values measured within 12 hours of each other in patients with SCD treated at the UI-Health from 2015-2017 were collected. A total of 28 INR pairs were used to form a discovery cohort. A cohort of non-SCD African American (AA) patients with POC-INR and CL-INR values measured within 12 hours who were treated at UIC-Health during the same period were utilized as a control group. Patient demographic and clinical characteristics were recorded to calculate a correction factor. Additional 28 POC- and CL-INR pairs in patients with SCD were used to form a validation cohort. Descriptive statistics, Kruskal-Wallis test, Chi-square test, and linear regression were used for data analysis. The study was approved by the UIC Institutional Review Board (protocol #2020-0191).
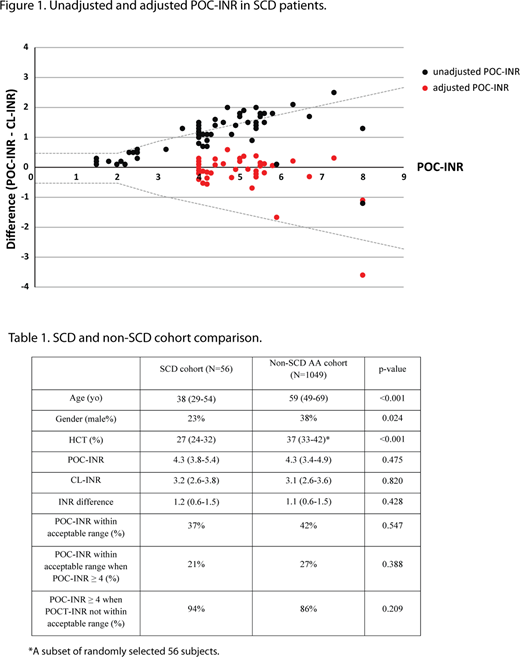
Results: In the discovery cohort with 100% AA patients, POC-INR in an acceptable range of the CL-INR, defined as an INR difference within ±0.5 INR of CL-INR when POC-INR < 2 or ±30% of CL-INR when POC-INR ≥ 2 (4), was present in 6 of 7 (86%) of patients when INR < 4 compared to 5 of 21 (24%) when INR ≥ 4. For POC-INR ≥ 4, a correction factor of 0.7 was derived using a linear regression model (95%CI: 0.685-0.752, P<0.001, R square: 0.991), which significantly improved the in-range POC-INR from 24% to 100% in the discovery cohort (P<0.001). In the validation cohort, the in-range POC-INR increased from 19% to 95% (P<0.001) after applying the correction factor of 0.7 (Figure 1). When compared to the non-SCD AA cohort, the patients with SCD were younger (38 vs 59 years, P<0.001) and more anemic (HCT 27% vs 37%, P<0.001). However, there was no significant difference in the in-range POC-INR percentage (37% vs 42%, P = 0.547) (Table 1). The correction factor for POC-INR ≥ 4 in the non-SCD AA cohort was the same as the SCD cohort as 0.7.
Summary: POC-INR over-estimates a simultaneous CL-INR when POC-INR ≥ 4 in patients with SCD, and a correction factor significantly improved the agreement with CL-INR. Despite the difference in anemia, the accuracy of POC-INR and correction factor were similar between SCD patients and non-SCD AA patients. An institution-specific correction factor for POC-INR ≥ 4 should be applied similarly to both SCD and non-SCD patients.
Reference:
1. R. W. Hoel et al., Correlation of point-of-care International Normalized Ratio to laboratory International Normalized Ratio in hemodialysis patients taking warfarin. Clin J Am Soc Nephrol4, 99-104 (2009).
2. C. E. DeRemer, B. McMichael, H. N. Young, Warfarin Patients With Anemia Show Trend of Out-of-Range International Normalized Ratio Frequency With Point-of-Care Testing in an Anticoagulation Clinic. J Pharm Pract32, 499-502 (2019)
3. A. Srisuwananukorn et al., Clinical, laboratory, and genetic risk factors for thrombosis in sickle cell disease. Blood Adv4, 1978-1986 (2020).
4. W. Plesch et al., Results of the performance verification of the CoaguChek XS system. Thromb Res123, 381-389 (2008).
Gordeuk:CSL Behring: Consultancy, Research Funding; Global Blood Therapeutics: Consultancy, Research Funding; Imara: Research Funding; Ironwood: Research Funding; Novartis: Consultancy. Saraf:Novartis, Global Blood Therapeutics: Membership on an entity's Board of Directors or advisory committees; Global Blood Therapeutics: Membership on an entity's Board of Directors or advisory committees, Other: Advisory Boards, Speakers Bureau; Pfizer, Global Blood Therapeutics, Novartis: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal